Evaluation of the In vitro Antimycobacterial Activities of Some Nigerian Medicinal Plants
Main Article Content
Abstract
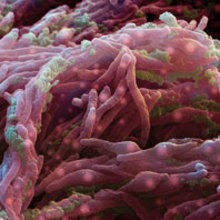
Various strategies which include the use of herbal medicines are be considered to reduce the burden and impact of tuberculosis and leprosy in Nigeria. Extracts obtained from four medicinal plants namely Rosary pea (Abrus precatorius), Hare’s bean (Desmodium ramosissimum), Stonebreaker (Phyllanthus amarus) and Sweet-broom (Scoparia dulcis) were screened for their antimycobacterial activities against Mycobacterium bovis (BCG) strain using the broth micro dilution method. Phytochemical analysis of the extracts was evaluated using standard techniques. All the extracts were active with varying minimum inhibitory concentrations (MICs). The methanol extract of Phyllanthus amarus gave the most potent inhibitory effect with the same Minimum Inhibitory Concentration (M.I.C.) and Minimum Bactericidal Concentration of 62.5μg/ml and 62.5μg/ml respectively. Phytochemical screening of the extracts indicated the presence of alkaloids, saponins, tannins and terpenoids for all the extracts. The result of this investigation provides scientific support for the ethno-medicinal uses of some of these plants for the management of mycobacterial infections. The methanol extract of P. amarus extract merits further investigation in order to obtain pure compounds that can serve as lead in the development of antimycobacterial drugs.
Metrics
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
References
Khandelwal S. and Dubey W. Overview of Mycobacterium: A Review. European J. Molecular and Clinical Med. 2020; 7 (11): 6198-6213
López-Roa P, Esteban J, Muñoz-Egea M.-C. Updated Review on the Mechanisms of Pathogenicity in Mycobacterium abscessus, a Rapidly Growing Emerging Pathogen. Microorganisms. 2023; 11: 90-98.
KNVC. Tuberculosis Foundation Annual Report 2023. Nigeria: start of the challenge TB project. [Online]. 2024[cited 2024 D March 10]. Available from: www.kncvtbc.org/en/project/nigeria-start-of-the-challenge-tb-project/.
Dahiru T, Abdullahi SH, van Knippenberg K, Taalb A, Schoenmakersb A, Bodunde DJ, de Bruijne N, Msheliza S, Ekeke N, Eze C, Chukuma A, Peters A. Leprosy: capacity in health facilities and among health workers: A baseline survey in Nigeria. Leprosy Rev. 2023; 94: 317–331
Kwaghe AV, Umeokonkwo CD, Aworh MK. Evaluation of the national tuberculosis surveillance and response systems, 2018 to 2019: National Tuberculosis, Leprosy and Buruli Ulcer Control Programme, Abuja, Nigeria. Pan African Medical J. 2020; 35:54.
Bendre AD, Peters PJ, Kumar J. Tuberculosis: Past, present and future of the treatment and drug discovery research. Current Res. in Pharmacol & Drug Discovery. 2021; 2: 1-9.
Riccardi G, Pasca MR. Trends in discovery of new drugs for tuberculosis therapy. J. Antibiotics (Tokyo) 2014; 67:655– 659.
Adepoju P. Nigeria's widening tuberculosis gap. The Lancet Infectious Diseases. 2020; 20(1): 29.
Odume B, Sheshi M, Chukwuogo O, Sani U, Ogbudebe C, Aniwada E, Emperor U, Nongo D, Eneogu R, Oyelaran O, Efo E, Dare D, Anyaike C. Drug resistant tuberculosis treatment service alignment with health seeking behaviour in selected states in Nigeria. J. Public Health and Epidemiol. 2023; 15(3): 158-165.
Ogoamaka C, Bethrand O, Lotanna U, Chidubem O, Sani, U, Nkiru N, Mamman B, Daniel E.; Chijioke O, Oloruntobi N, Austin I, Debby N, Rupert E, Omosalewa O, Emperor U, Chukwuma A. The TB Surge intervention: an optimized approach to TB case-finding in Nigeria. Public Health Action. 2023; 13, (4):136-141.
Oke G, Nsofor I, Abubakar B, Utaka EN. Experience of people living with leprosy at leprosy settlements in Nigeria. Public Health Challenges. 2024; 3(2): 1-14 DOI: 10.1002/puh2.171.
Anochie PI, Ndingkokhar B, Bueno J, Anyiam FE, Ossai-Chidi LN, Onyeneke EC, Onyeozirila AC. African Medicinal Plants that Can Control or Cure Tuberculosis. Inter J. Pharm Sci Development Res. 2018; 4(1):001-008.
Sundar RD, Settu S, Shankar S. et al. Potential medicinal plants to treat leprosy—A review. Res J. Pharm Technol. 2018; 11 (2 ): 813 – 821 .
Okonkwo OB, Afieroho OE, Bimba JS, Eliya TT, Osuji, AU, Abo KA. A triterpene ketone from an anti-mycobacterial tuberculosis chromatography eluate from the n-hexane fraction of the fruits of Harungana madagascariensis Lam. Ex Poiret (Hypericaceae). GSC Biol and Pharm Sci. 2022; 18(02): 259–267.
Singh A, Venugopala KN, Pillay M, Shode F, Coovadia Y, Odhav B. Antimycobacterial activity of aqueous and methanol extracts of nine plants against Mycobacterium bacteria. Trop J. of Pharm Res. 2021; 20(4):1596-5996.
Oloya B, Namukobe J, Ssengooba W, Afayoa M, Byamukama, R. Phytochemical screening, antimycobacterial activity and acute toxicity of crude extracts of selected medicinal plant species used locally in the treatment of tuberculosis in Uganda. Trop Med and Health. 2022; 50(16): 1-13.
Mpeirwe M, Taremwa IM, Orikiriza P, Ogwang PE, Ssesazi D, Bazira J. Anti-Mycobacterial Activity of Medicinal Plant Extracts Used in the Treatment of Tuberculosis by Traditional Medicine Practitioners in Uganda. Pharmacol & Pharmacy. 2023; 14:33-42.
Ramadwa TE, Awouafack MD, Sonopo MS, Eloff JN. Antibacterial and Antimycobacterial Activity of Crude Extracts, Fractions, and Isolated Compounds From Leaves of Sneezewood, Ptaeroxylon obliquum (Rutaceae). Natural Product Comm. 2019; 14(9): 1–7
Achika JI, Yusuf AJ, Ayo RG, Liman DU. Flavonoids from Nigerian indigenous medicinal plants and their bioactivities: A review. Phytomedicine Plus. 2023; 3(2): 1-34.
Gautam S, Qureshi KA, Jameel-Pasha SB, Dhanasekaran S, Aspatwar A, Parkkila S, Alanazi S, Atiya A, Khan MMU, Venugopal D. Medicinal Plants as Therapeutic Alternatives to Combat Mycobacterium tuberculosis: A Comprehensive Review. Antibiotics. 2023; 12: 541-559.
Ugboko HU, Nwinyi OC, Oranusi SU, Fatoki TH, Omonhinmin CA. Antimicrobial Importance of Medicinal Plants in Nigeria. Scientific World J. 2020; Article ID 7059323, 10 pp
Alli AI, Ehinmidu JO, Ibrahim YKE. Preliminary Phytochemical Screening and Antimicrobial Activities Of Some Medicinal Plants Used In Ebiraland. Bayero J. of Pure and Applied Sci. 2011; 4(1): 10 – 16.
Jethva KD, Bhatt DR, Zaveri MN. Antimycobacterial screening of selected medicinal plants against Mycobacterium tuberculosis H37Rv using agar dilution method and the microplate resazurin assay. Inter J. Mycobacteriology. 2020; 9:150-5.
Shaikh JR, Patil MK. Qualitative tests for preliminary phytochemical screening: An overview. Inter J. of Chem Studies. 2020; 8(2): 603-608.
Li X, Jin G, Yang J, Li Y, Wei P, Zhang L. Epidemiological characteristics of leprosy during the period 2005–2020: A retrospective study based on the Chinese surveillance system. Frontiers in Public Health. 2023; 10:991828.
Olatunji KT, Aliyu A, Ya’aba YM, Shehu B, Oladosu P. Phytochemical analysis and antituberculosis activity of extracts of Detarium senegalense bark and root. J. Advances in Microbiol. 2021; 21: 44-50
Kasim IS, Ibrahim YKE, Onoalapo JA, Ibrahim K, Oladosu P, Ibekwe NN, Obi AP. Synergistic activity of Tetrapleura tetraptera and Abrus precatorius fractions extract against Streptococcus pneumoniae and Mycobacterium tuberculosis. J. Phytomed and Therapeutics. 2023; 22(1), 1045- 1057.
Newton SM, Lau C, Gurcha SS, Besra GS, Wright CW. The evaluation of forty-three plant species for in vitro antimycobacterial activities; isolation of active constituents from Psoralea corylifolia and Sanguinaria canadensis. J. Ethnopharmacol. 2002; 79(1):57-67.
Soundhari C, Rajarajan S. In vitro s creening of lyophilised extracts of Alpinia galanga L and Oldenlandia umbellata L. for antimycobacterial activity. Inter J. of Biol and Pharm Res. 2013; 4(6):427-432.
Mohamad S, Ismail NN, Parumasivam T, Ibrahim P, Osman H, Wahab HA. Antituberculosis activity, phytochemical identification of Costus speciosus (J. Koenig) Sm., Cymbopogon citratus (DC. Ex Nees)Stapf., and Tabernaemontana coronaria (L.)Willd. and their effects on the growth kinetics and cellular integrity of Mycobacterium tuberculosis H37Rv. BMC Compl and Altern Med. 2018;18, (5):1-14.
Saludes JP, Garson MJ, Franzblau SG, Aguinaldo AM. Antitubercular constituents from the hexane fraction of Morinda citrifolia Linn. (Rubiaceae). Phytotherapy Res. 2002; 16:683–685
Ibobo , GO, Okpoghono, J, Onyesom, I. . Polyphenol Profile and Antioxidant Properties of Various Solvent Fractions of Phyllanthus Amarus. Trop J Phytochem Pharm. Sci. 2024; 3(3): 246-253 http://www.doi.org/10.26538/tjpps/v3i3.6
Mangwani N, Singh PK, Kumar V. Medicinal plants: Adjunct treatment to tuberculosis chemotherapy to prevent hepatic damage. J. Ayurveda and Integrated Med. 2019; 11(4): 522-28.
Yadav M, Sharma P. Plant-derived Molecules for the Treatment of Tuberculosis: A Review. Iraqi J. Pharm Sci. 2022; 31(2):1-13.